This Is Our Story

Expert Virtual Assistant
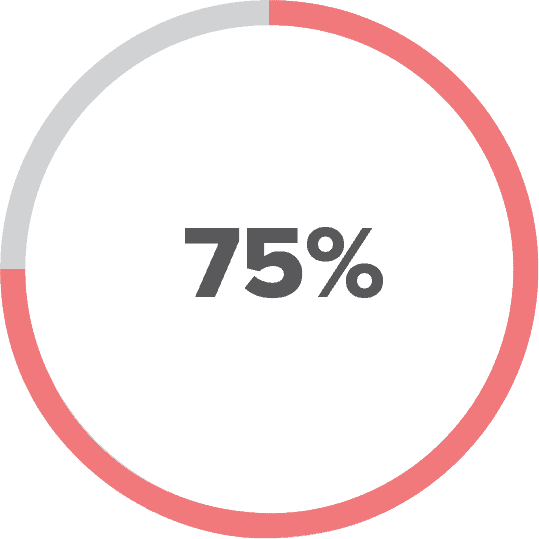
The expert virtual assistant (EVA) uses cloud-based software to compress EMR time by as much as 75%. Stanford recently released data showing that the average outpatient visit required 18 minutes of EMR “screen time” to complete 11 minutes of clinical “face time.” EVA presents an electronic questionnaire to interview patients through their personal devices or in the provider’s office. This dynamic questionnaire generates the bulk of the medical record. Rules-based algorithms apply artificial intelligence (AI) to interpret the data and present a preliminary document to the patient and provider:
- The patient dashboard presents an overall “health score” to approximate global wellness.
- “Open notes” format enhances shared-decision making and informed consent.
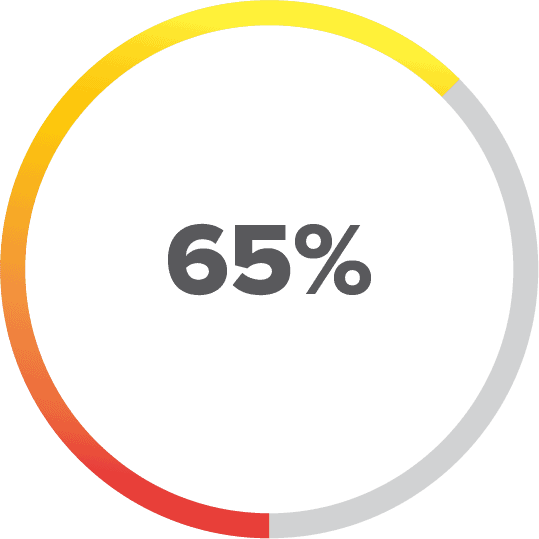
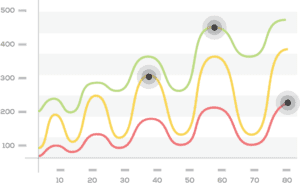
- Graphic displays present patient data in clear, concise terms.
- Providers and patients share this graphic data for clarity and education.
- A complete history and review of systems are recorded and subjected to rules algorithms for enhanced clinical decision-making.
- Laboratory data is integrated into the AI for further refinement of clinical decision-making.
- Embedded multidisciplinary questionnaires produce a multi-specialty functional assessment.
- Preliminary reports are finalized by providers after an in-depth interview and physical examination.
- Ongoing access to the provider and patient produces complete transparency and participation.
- High-efficiency scheduling, E-prescribing, and invoicing are integrated into the system.
Providers and healthcare staff may engage EVA before face-to-face patient contact for rapid assessment of overall health status, chief complaint(s), and other history and systems reviews. EVA interprets and highlights significant positive and negative historical findings for the preliminary medical record. The provider follows up with focused questions, laboratory studies, and physical examinations for final diagnoses. EVA presents patients to providers for final evaluation and treatment. Scheduling, prescribing, billing, patient communication, and other basic functions are mindfully integrated into EVA’s process. EVA saves time and improves care through patient participation and rules-based AI.
Background
Thousands of years ago, Hippocrates and the ancient Greeks developed a medical system that respected the inter-relationship of nutrition, psychology, anatomy, and lifestyle. The body’s innate ability for self-healing was supported through a prescription of diet, exercise, social support, and symptomatic relief.

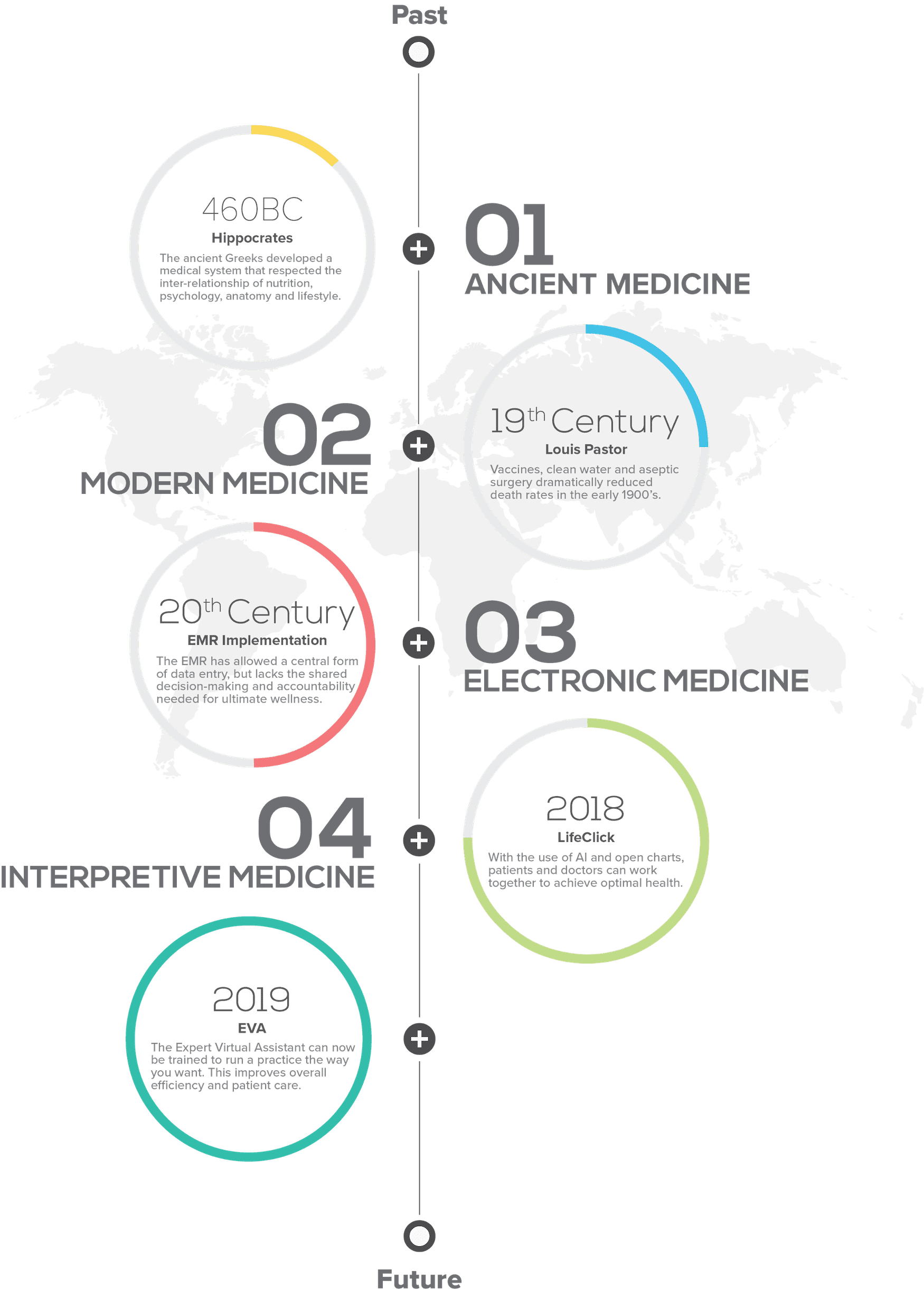
The primary function (of the EMR) was to enhance billing, not to build a physician-patient relationship. Our productivity went down 25 percent. 2
– Dr. Michael Ciampi
Electronic medical records and electronic health records share the same fundamental flaw. Systems designed to record disease codes for insurance reimbursement are destined to fail. Personalized care, shared decision-making, and accountability require a comprehensive re-framing of the approach to medicine. Patients as partners in the process of data acquisition and electronic systems as intelligent partners for interpretation present a more logical progression from the ancient foundations of medicine until today.

EVA is built on the health and wellness model, encouraging individual responsibility through required participation in data acquisition. Interpretive logic underlies every step of the internal processing of this data, including history, symptoms, and objective laboratory data. The scope of these algorithms exceeds the average processing ability of a practitioner in day-to-day practice. An enhanced experience is shared by patient and provider alike as collected, and interpreted data is presented for mutual consideration. Treatment plans encompass diet, nutrition, lifestyle, psychology, and modern medical intervention. None of the ancient treasures of Hippocratic wisdom is sacrificed at the altar of expediency. The cornerstone of the patient-centered medical home is laid by the one with the most to gain and to lose. Third-party influence is removed from the process at its core and placed appropriately in the terminal component of the process during invoicing and payment.
The Empowered Patient
An empowered patient has control over the management of their condition in daily life. They take action to improve the quality of their life and have the necessary knowledge, skills,attitudes and self-awareness to adjust their behaviour and to work in partnership with others where necessary, to achieve optimal well-being. 3
– Project EMPATHiE
EVA empowers patients by enlisting their participation from the initial generation of the medical record to the final development of a comprehensive care plan. Active participation is encouraged and reinforced throughout the health interview process. Patients are empowered with an enhanced awareness of their symptoms and medical history as valuable data points. With repetition and training, the EVA’s system-based logic allows for simultaneous targeted data acquisition and patient education. EVA conducts structured interviews to demonstrate clinical problem-solving models to patients while recording/interpreting chief complaint(s) and pertinent historical and laboratory data. EVA provides round-the-clock availability allowing patients to input and update data from a broad range of resources:
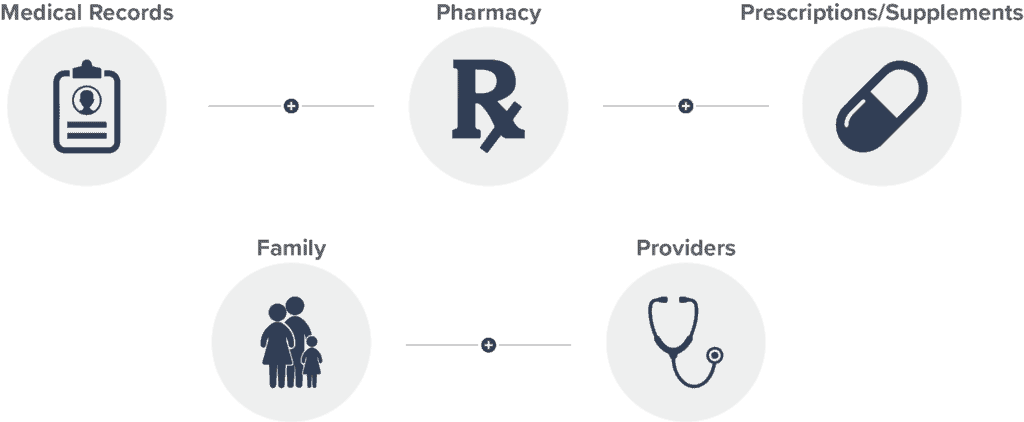
Patient empowerment is central to the role of EVA. Patient-driven health and wellness options and lifestyle interventions complement traditional medical treatment. Opportunities for patient engagement are suggested by EVA and approved by the patient and provider.
Accelerating Documentation
-
Time spent on direct patient care.
-
Everything Else
-
38% EMR documentation and review
-
19% Administrative tasks related to insurance or billing
-
11% EMR review of tests, medications, or other orders
-
6% Clinical planning and logistics
And this doesn’t include:
-
Self-reported 1 to 2 hours of evening time spent on administrative tasks
-
39% of “patient-facing time” spent in the EMR 4
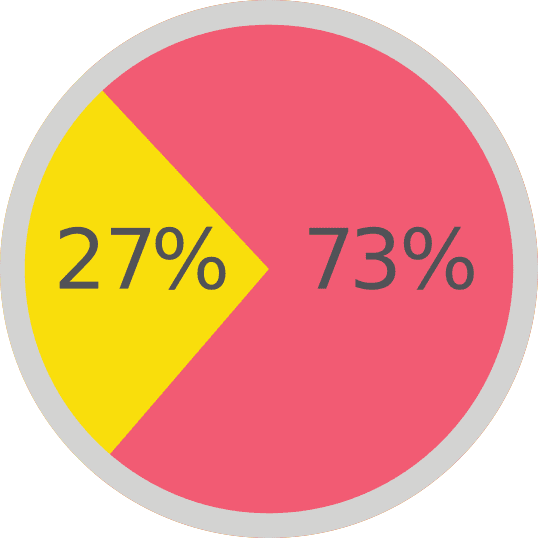
Electronic medical records (EMRs) are considered the number one source of “burn-out” in medicine today. Recent studies show that 19 of 31 minutes spent on a patient’s visit are occupied with documentation in existing EMRs.5 Most EMRs have been built with a focus on compliance with government regulations and insurance reimbursement. This results in an inevitable reduction in the percentage of the system designed to facilitate patient care. EVA is focused on a comprehensive evaluation of the roots of illness with participative patient care as leverage to produce improved outcomes. Regulatory requirements and reimbursement issues are deemphasized in favor of enhanced patient care and ease of documentation. This fundamental reorientation decreases “screen time” by as much as 75%.
EVA accelerates documentation by recruiting the patient as a scribe, starting with their chief complaint. Different prompts guide in-depth descriptions of the chief complaint and an extensive history and review of systems. EVA employs a tiered questioning system to explore significant findings in greater depth. EVA will drill down to sub-questions and sub-sub-questions to delineate specific possible problems if a response suggests further investigation. This systematic, progressively detailed questioning saves substantial documentation time. Answers to each question are converted from everyday language to medical terminology to comply with standard medical record-keeping.
Improving Outcomes
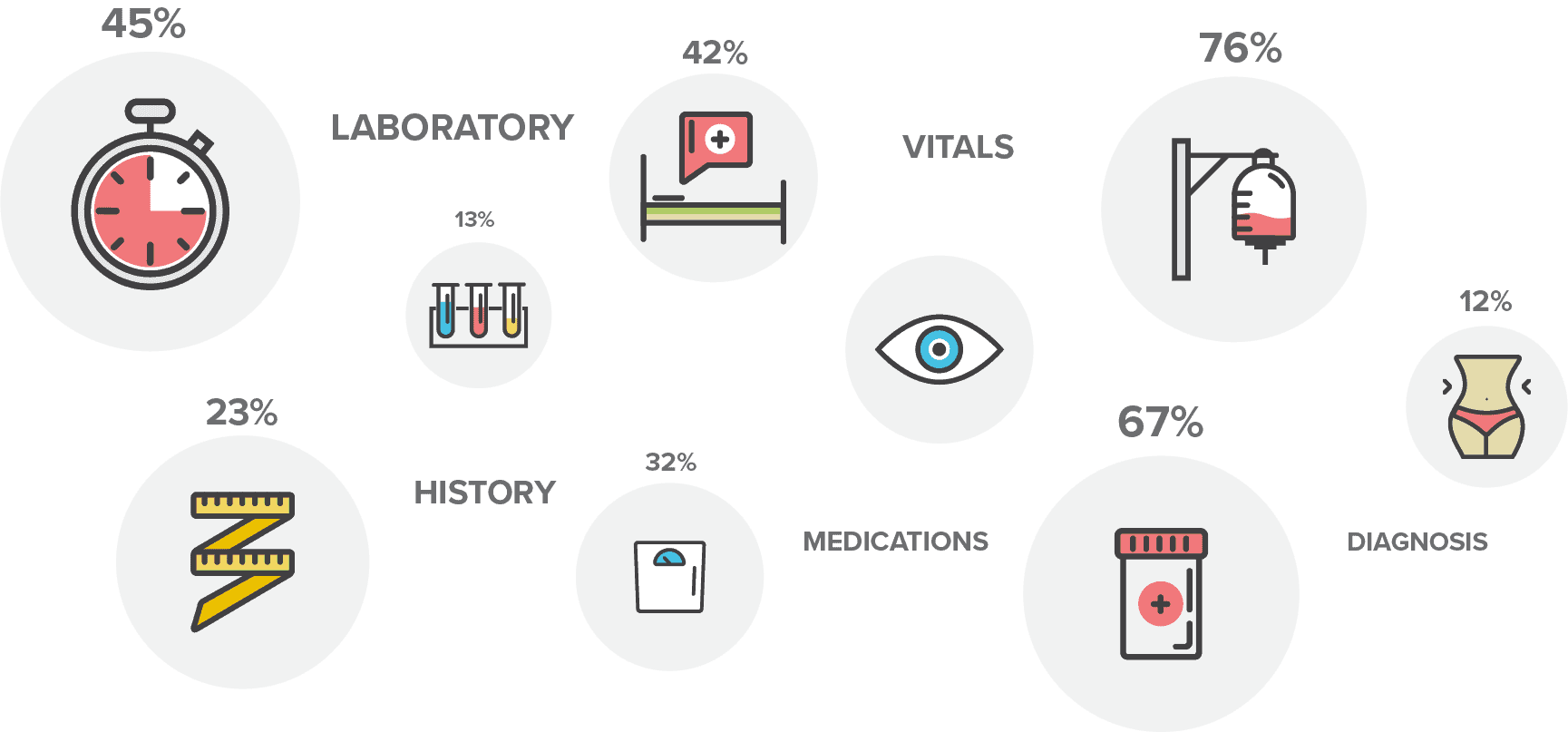
EVA improves outcomes by interpreting the complaint, history, and review of systems from the perspective of multiple disciplines. Questions derived from validated questionnaires are cross-referenced from a broad range of specialties:
- Endocrinology
- Psychiatry
- Gastroenterology
- Allergy and Immunology
- Neurology
- Orthopedics
- Cardiology
- Hematology and Oncology 200
- Preventive Medicine
- Urology
- Gynecology
Patient-entered responses (answers) are applied to a set of rules for each functional area. These rules calculate the likelihood that any combination of symptoms may result from compromised function in a body system. For example, the combination of dizziness upon standing, the tendency to feel cooler than others, and salt craving indicate a high likelihood of adrenal stress or imbalance. A single response may be applied to multiple rules to determine if multiple functional systems are simultaneously impacted. Responses are assigned a positive or negative predictive value based on clinical experience and repeated testing of over 50,000 interviews. The probability of system failure is calculated from patient-generated data and then cross-checked against available laboratory values. Preliminary scores are graphed and presented for further evaluation by providers. Improved outcomes result from a more thorough understanding of the causes of symptoms and functional disturbances. Seeing the “big picture” spelled out before beginning the time-intensive work of collecting data face-to-face saves hours and money.
Artificial Intelligence/Algorithms
Artificial intelligence (AI) can loosely be defined as the ability of a machine (computer) to think or create solutions to problems. EVA applies artificial intelligence through algorithms in the interview process (Phase I). First-level questions will trigger second and third-level questions to follow a line of reasoning to improve diagnostic accuracy. Second and third-level questions will not be presented by EVA if they are unlikely to improve diagnostic accuracy. This reduces the number of unnecessary questions given to any patient.
01
PHASE
EVA applies artificial intelligence through algorithms in the interview process.
03
PHASE
Rules-based algorithms interpret the answers to intertwined question sets to initiate the process of problem-solving.

02
PHASE
Laboratory evaluations are imported through an HL7 bridge.
04
PHASE
Diagnosis results in disease avoidance, risk reduction, and good health care.
Further rules-based algorithms (Phase II) interpret the answers to intertwined question sets (symptom clusters) to initiate the process of problem-solving. These algorithms create a cumulative score to determine the probability of dysfunction in specified health categories. Questions extrapolated from validated instruments are assigned to each health category and weighted according to the clinical significance of each response. The same question is frequently applied to widely divergent health and wellness fields. For instance, a question about headaches may be scored for its impact on psychiatry, endocrinology, toxicology, and structural medicine. A “whole-patient” evaluation is generated and documented at the first step (Phase I) of EVA’s engagement.
Validated questionnaires are commonly used in medical practice to organize patient data collection and assist in the development of accurate diagnoses. Patient frustration with excessive and/or repetitive paperwork is legendary. By layering dozens of validated instruments within EVA, repetition is minimized. EVA creates a straightforward method for documenting, storing, and retrieving relevant data. Response to drug recalls, new treatment options, and population studies are performed with these readily accessible databases.
Laboratory evaluations, imported through an HL7 bridge, complete the interpretive function of EVA (Phase III). Symptom clusters are subjected to rules derived from the questionnaire and are initially scored separately from lab values. Preliminary findings based solely on the interview provide highly predictive outputs that can be useful for screening and treating many conditions at a very low cost. Laboratory studies rule in or rule out diagnoses with a separate layer of rules-based algorithms to complement the phase I interview process. Diagnoses based on lab data alone frequently miss the nuanced findings of a sophisticated interview. Early identification of subtle dysfunction requires a detailed interview and laboratory investigation. Disease avoidance, risk reduction, and good health care result from the integration of EVA (Phase IV).
Patient Involvement

In contrast, EVA engages the patient in data collection before a visit with minimal update activity during clinical interactions. A large shared screen is utilized by EVA to finalize records, review laboratory data, and update prescriptions and other treatment recommendations with the patient. The “open notes” format allows entire visits with high complexity to be completed in cooperation on a shared screen.
EVA is appreciated within the context of current depersonalizing office visits driven by the demands of an EMR. EVA’s focus on patient education and participation enhances informed consent and compliance with treatment protocols. Graphic displays highlight overall health status, individual system status, and laboratory trends. Heightened awareness and an increased sense of control support shared decision-making from an informed perspective.
EVA uses an “Open Notes” format to allow patients to view their entire medical record. Sharing the medical record has been shown to improve compliance with treatment, increase safety, strengthen the relationship, and build trust between patient and provider. EVA shares each step of the evaluation and integrates the provider’s input through secure text messaging to clarify lab findings, outside consultations, and patient-uploaded records from other sources. Shared decision-making becomes a reality in the context of “Open Notes.”
Regulatory Compliance
Regulatory paperwork complicates efficient patient care. EVA presents informed consent, HIPAA, medication contracts, and other necessary forms systematically and less tediously. Patients have access to all signed materials before visits to allow genuinely informed consent. EVA retains copies of signed forms for permanent access by the patient and provider.
Citations
-
http://med.stanford.edu/content/dam/sm/ehr/docu- ments/SM-EHR-White-Papers_v12.pdf
-
http://www.governing.com/topics/health-human-ser- vices/gov-doctors-electronic-health-records.html
-
https://ec.europa.eu/health//sites/health/files/major_ chronic_diseases/docs/ev_20160421_co04_en.pdf
-
https://gisthealthcare.com/physician-burnout-noth- ing-personal/
-
http://med.stanford.edu/content/dam/sm/ehr/docu- ments/SM-EHR-White-Papers_v12.pdf